The New Yorker published an article in the summer of 2021 comparing public health policy in Costa Rica to that of the United States. The result is clear: in Costa Rica, where public health is considered a priority, people live longer. Certainly not as many as in Switzerland, where the number of centenarians is exploding, but enough to make one wonder. How did this country manage to surpass North America?
Thanks to a national policy since the 1970s, which defined a strategic plan to expand the coverage of care provided by the social security system. Costa Rica also developed a rural health program, which extended the type of medical services that were available in the cities to the rest of the country. This is remarkable. However, it is questionable whether longevity is really the overriding goal, as illustrated by the debates on quality of life. As a research (whether basic, translational or clinical) and teaching institution, we do not have the authority to set national public health policy. However, we can contribute to it, in particular through our privileged partnership with institutions such as the CHUV and Unisanté.
Without calling into question our cutting-edge activities in the treatment of serious diseases that aim to prolong the life expectancy of patients, we can ask ourselves broader questions about health: how can our research and teaching contribute to a better quality of life? Are we moving in the right direction? At what levels is it possible to act? Is health an individual or collective matter? Today, I would like to try to find the beginning of an answer by exploring three "determinants of health" with researchers from UNIL.
The first is sport, and more generally physical activity. This is an intuitive hypothesis that will, a priori, make many people agree! However, Aaron Baggish, Professor at the Faculty of Biology and Medicine and Chief of Cardiology at the CHUV, goes further: of all the actions an individual can take to stay healthy, practicing sports is by far the most important - combined, of course, with a healthy diet and not smoking. 150 minutes of moderate exercise or 75 minutes of intense exercise per week is enough to drastically improve the quality of life. This is the first step to take in terms of public health. At the individual level, every little step counts: walking more, taking the stairs instead of the elevator... any effort, no matter how small, is better than nothing, regardless of age or previous health status. Moreover, according to him, physical activity smoothes out socio-economic barriers because it is free, unlike pharmaceuticals, which only a portion of the population can afford. However, exercise must be individualized. While we know the use of drugs, their dosage, side effects and restrictions of use, we know nothing about sport. However, an asthma patient should logically be advised to do different types of exercise than someone with back problems, for example. We are all unique, and should be able to follow a perfectly adapted "dose" - just like a medical prescription. That's where Professor Baggish's research comes in. Within five to 10 years, he hopes to have qualified and quantified the effects of different "doses" of sport, and then plans to develop a data platform that allows people to get personalized information to choose the most appropriate physical activity. Next, it will be a matter of convincing government decision-makers, perhaps even health insurers, that an incentive policy could save them millions per year - and not just by offering bonuses for cross-country ski pass holders... The creation of safe outdoor exercise paths, the provision of indoor sports facilities in winter, the installation of showers, the reorganization of working hours, the inclusion of physical activity in professional CVs, or even financial compensation (such as reductions in meal prices on presentation of a pedometer) - there are many possible incentives, and they must also come from above. Without active stimulation from the environment, the efforts of each individual are doomed to failure.
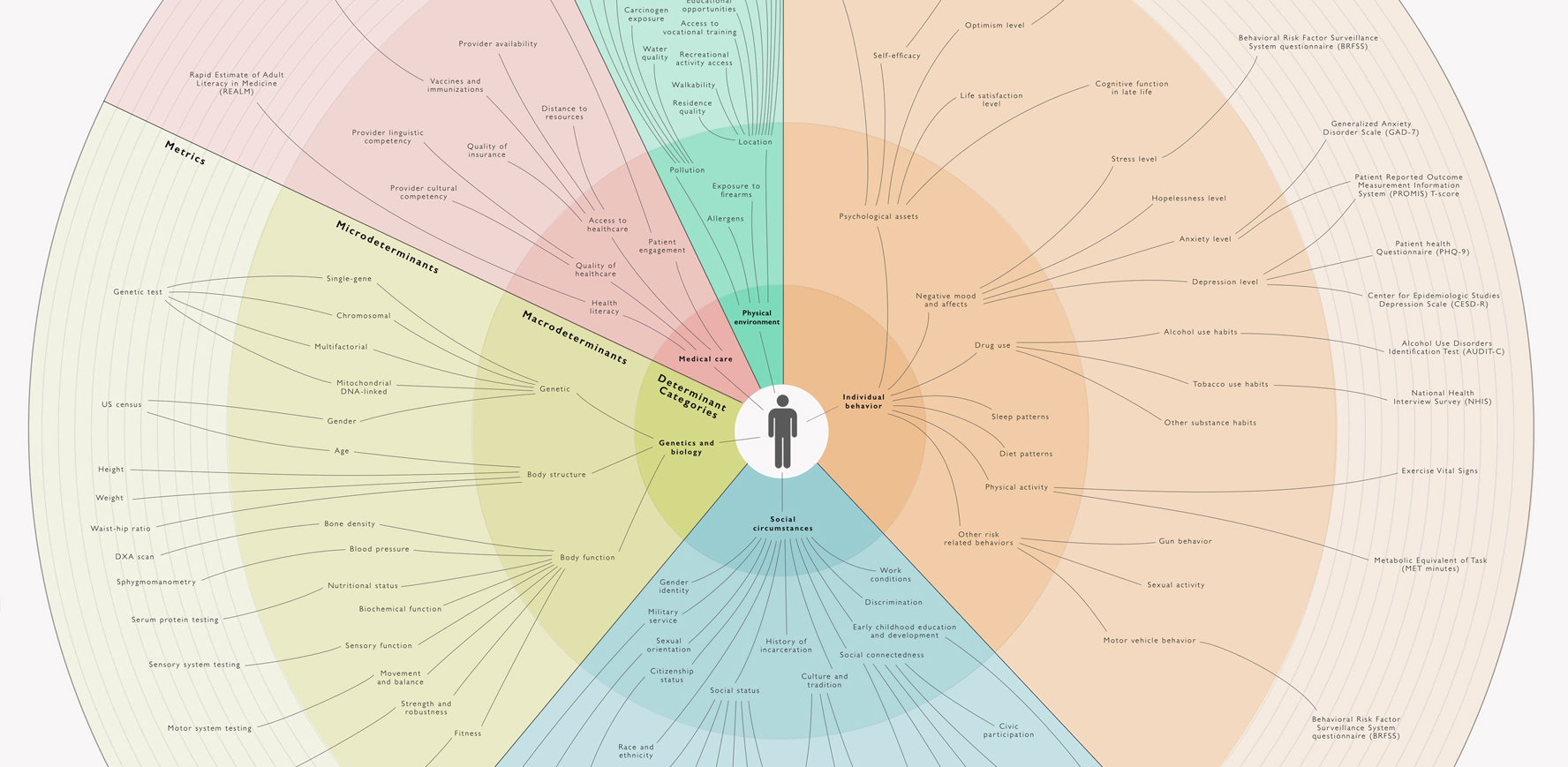
For the social science experts of UNIL, Nolwenn Bühler, anthropologist of medicine and health, and Francesco Panese, Professor of social studies of medicine and science, individual behavior remains a predominant determinant of health (36% according to the attached diagram). For this reason, historically, governments have often targeted individuals to implement health policies through behavioral changes: teaching people to brush their teeth, to air, or to avoid giving alcohol to children.
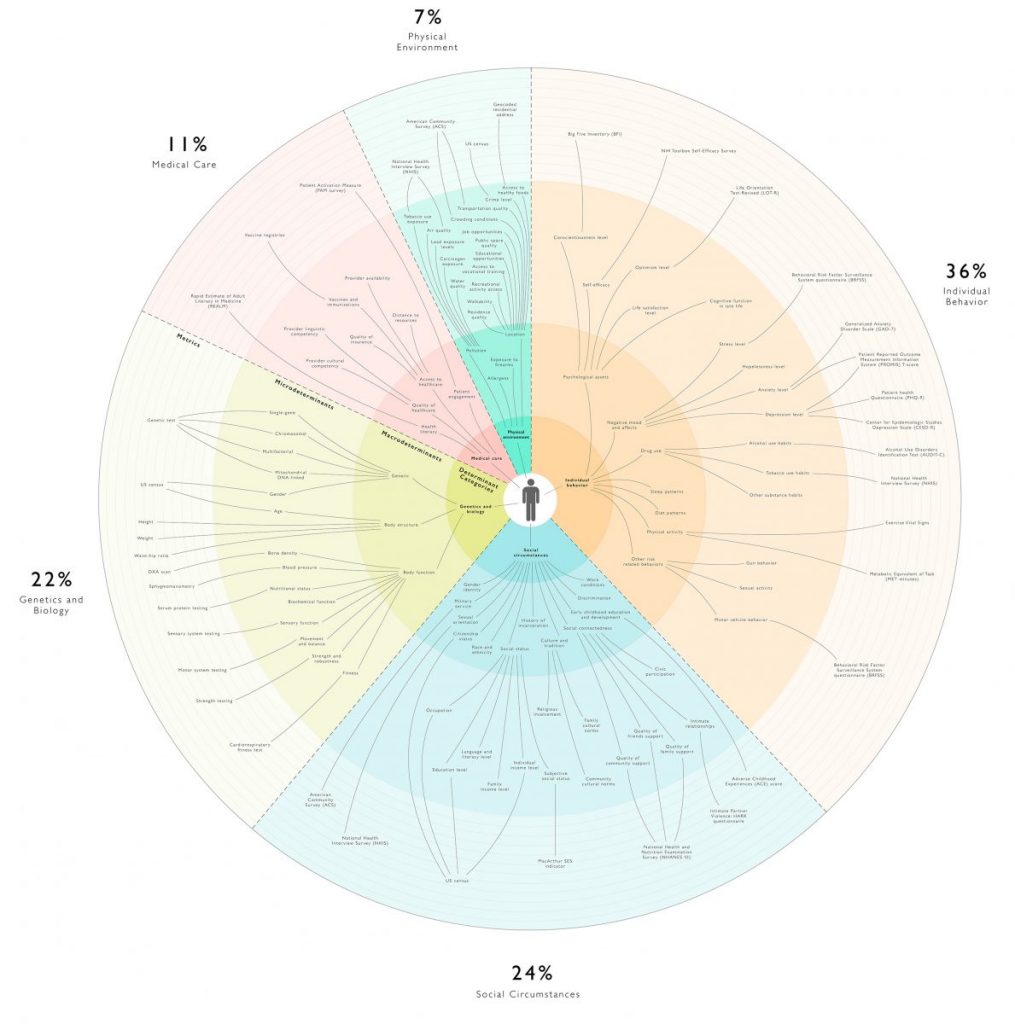
The trend to individualize prevention measures continues today. However, while this may emphasize individual choices, it can also contribute to the stigmatization of risky behaviour. We know that such "pedagogical" measures are not enough, especially because they neglect socio-environmental factors. Is it really relevant to encourage a person to go jogging in an ultra-polluted city, knowing that he or she may absorb a large quantity of toxins in the process? Should we push people to eat better by consuming healthier but more expensive products that only increase inequalities? Studies show that living conditions and social status, such as gender, ethnicity, sexual and emotional orientation, income or education level, are fundamental to health (24%) - much more so, contrary to popular belief, than medical care (11%). In order to account for these elements that are beyond the direct reach of individuals, the notion of "health determinant" is becoming more refined and complex. For example, the notion of "modulator" can be introduced to reflect the way in which the biological and the social interact in a dynamic way throughout the life cycle. Improving health today would therefore require a return to a more contextual conception, which has been eclipsed by the rise of genetics and the biomedicalization of public health. However, Hippocrates (460-377 BC), in his treatise On Airs, Waters and Places, already advised medical practitioners to closely observe the quality of the water and soil in the cities where they came to practice. In the 19th century, it was known that it was necessary to start by cleaning up the places and draining the swamps in order to implement a long-term health policy...
It is therefore a holistic approach and a resocialization of health that should take precedence, for example by using the concept of the exposome. Developed in epidemiology, this concept encompasses the totality of exposures to external (non-genetic) factors experienced by every human being from conception to death (including, for example, the political and economic system, working conditions or heavy metals and pollutants). But the task is arduous: how to develop and finance a system that manages to link such a mass of data, and this over the long term? Who decides on public health priorities, what to monitor and for what purpose? Is it the interest of the scientists, of the population or of the state authorities in charge of public health? Is the scientific evidence on the influence of social determinants sufficient when systemic measures depend on political will and the democratic agenda?
To answer these questions, Nolwenn Bühler conducted an ethnography of a population cohort carrying out a biomonitoring study and seeking to understand the impact of the environment on health. Defending a committed posture, she actively collaborates with physicians and public health researchers in order to strengthen the consideration of the social dimensions of health inequalities. In order to do so, it is important to initiate a fundamental reflection on the position and orientations of public health in Switzerland, as well as to incite the medical system to think in a syndromic way by bringing together elements that have been treated in silo until now (for example, as Francesco Panese explains, remembering that an epidemic such as AIDS or COVID is not a simple matter of health, but that factors of precariousness, lifestyle or sectors of activity play a crucial role in the propagation of the virus). In the long run, it would therefore be a matter of involving the decision-making bodies in order to refound a health policy in the law, which is now outdated.
Changing the legislation behind the health system is also the conclusion reached by Professor Valérie D'Acremont, a physician and epidemiologist, specialist in infectious diseases and tropical medicine, responsible for the Global and Environmental Health Sector at the University Centre for General Medicine and Public Health (Unisanté). His arguments are based on his own research specialty: climate change and its impact on health. In his view, it is imperative to work on three interconnected issues that alter our basic needs and reinforce each other:
- extreme climatic changes, such as heat waves (1,000 deaths per year in Switzerland, not counting the effects on agriculture) or floods (which impact water quality and migration)
- the collapse of biodiversity - the destruction of forests, intensive breeding and our ultra-liberal production system favor the emergence of new pathogens and their rapid dissemination
- pollution itself - water and soil contaminated by pesticides or endocrine disruptors lead to early cancers and sterility, micro-particles in the air trigger lung and artery diseases (3'000 deaths each year in our country).
All these imbalances also have an effect on our mental health (eco-anxiety, anxiety in case of conflict or migration). They affect our diet and increase social inequalities. Even if it does not necessarily feel impacted by these problems, Switzerland unfortunately does not escape them. Obesity (11% of the adult population), early cancers, increased heatstroke, infectious diseases such as tick-borne encephalitis, increasing cases of allergy or asthma, and above all cardiovascular diseases that create a fragile terrain in the event of a pandemic... Arboviruses (dengue fever, chikungunya, Zika) are approaching our borders, and we are not immune to permafrost collapses. Faced with this observation, the WHO asked countries to submit two roadmaps after the last COP27 so that they would consider, on the one hand, modifying their health systems to adapt to the emergence of new diseases and, on the other hand, decarbonizing them (they are currently very polluting in terms of CO2 emissions and soil contamination, especially because of drugs). For Valérie D'Acremont, one of the solutions would be to make the healthcare system much more sober by returning to a human-centered approach based on primary care medicine, and by reinforcing prevention (Switzerland holds the world record for consumption of energy and raw materials, mainly due to the ultra-technologicalization of medicine, but, for the same quality of care, Sweden consumes three times less). Such a transformation requires changes in legal frameworks and public health programs. For the time being, the Confederation has not responded to the WHO's call. But specific initiatives are multiplying at the local level, such as the Blue Walk (four women from the canton of Vaud, including Valérie D'Acremont and Julia Steinberger, Professor of societal issues related to the impact of climate change at the Institute of Geography and Sustainability of UNIL, are going to rally Geneva to Bern to raise awareness about the climate emergency). Collective actions, such as the health hamlets in France, which propose a new paradigm of holistic, democratic, social and ecological care, also give hope that things will change.
Sans être spécialiste, loin de là, il me semble donc clair que nous ne pourrons parvenir à améliorer notre santé future qu’à travers une double approche : au niveau privé, en priorisant le sommeil, l’activité physique, un environnement matériel et social le plus sain possible, une bonne nutrition et une médecine préventive de proximité, et, au niveau professionnel, en continuant à dialoguer entre chercheuses et chercheurs de nos sept facultés pour aider à recomposer ensemble une société où chacun·e puisse vivre mieux au quotidien, quelle que soit sa trajectoire – et pas uniquement en se félicitant de notre médaille d’or de la longévité !
Links
- La Suisse est la nouvelle championne de la longévité, Tribune de Genève 2023-29-01
- Costa Ricans Live Longer Than We Do. What’s the Secret? New-Yorker 2021-31-08
- Santé et environnement : vers une nouvelle approche globale
- Merrill Singer, Syndemics and the biosocial conception of health, The Lancet
- La Marche bleue